Unraveling Connections Between the Brain and Gut
MIT engineers have developed a new optogenetic technology that can manipulate the neurological connections between the brain and gut, potentially offering insights into the links between digestive health and neurological conditions.
The brain and the digestive tract are in constant communication, relaying signals that help to control feeding and other behaviors. This extensive communication network also influences our mental state and has been implicated in many neurological disorders.
MIT engineers have designed a new technology for probing those connections. Using fibers embedded with a variety of sensors, as well as light sources for optogenetic stimulation, the researchers have shown that they can control neural circuits connecting the gut and the brain, in mice.
In a new study, the researchers demonstrated that they could induce feelings of fullness or reward-seeking behavior in mice by manipulating cells of the intestine. In future work, they hope to explore some of the correlations that have been observed between digestive health and neurological conditions such as autism and Parkinson’s disease.
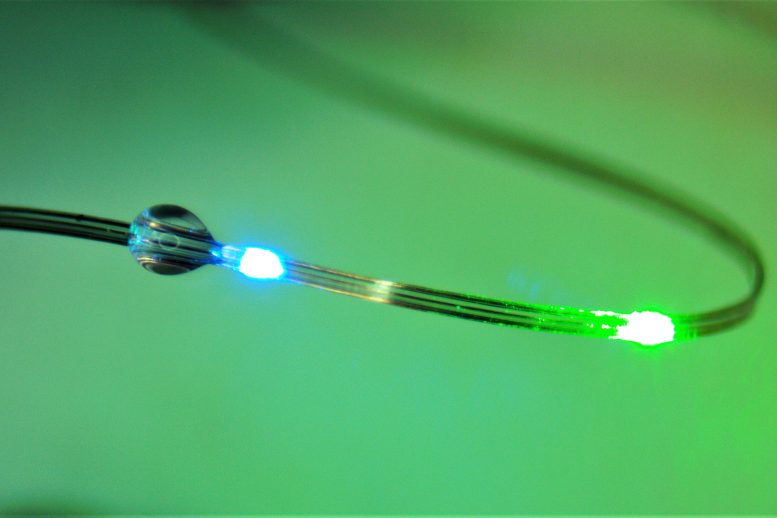
These flexible fibers, which are embedded with sensors and light sources, can be used to manipulate and monitor the connections between the brain and the digestive tract. Credit: Courtesy of the researchers
“The exciting thing here is that we now have technology that can drive gut function and behaviors such as feeding. More importantly, we have the ability to start accessing the crosstalk between the gut and the brain with the millisecond precision of optogenetics, and we can do it in behaving animals,” says Polina Anikeeva, the Matoula S. Salapatas Professor in Materials Science and Engineering, a professor of brain and cognitive sciences, director of the K. Lisa Yang Brain-Body Center, associate director of MIT’s Research Laboratory of Electronics, and a member of MIT’s McGovern Institute for Brain Research.
Anikeeva is the senior author of the new study, which was published on June 22 in the journal Nature Biotechnology. The paper’s lead authors are MIT graduate student Atharva Sahasrabudhe, Duke University postdoc Laura Rupprecht, MIT postdoc Sirma Orguc, and former MIT postdoc Tural Khudiyev.
The brain-body connection
Last year, the McGovern Institute launched the K. Lisa Yang Brain-Body Center to study the interplay between the brain and other organs of the body. Research at the center focuses on illuminating how these interactions help to shape behavior and overall health, with a goal of developing future therapies for a variety of diseases.
“There’s continuous, bidirectional crosstalk between the body and the brain,” Anikeeva says. “For a long time, we thought the brain is a tyrant that sends output into the organs and controls everything. But now we know there’s a lot of feedback back into the brain, and this feedback potentially controls some of the functions that we have previously attributed exclusively to the central neural control.”
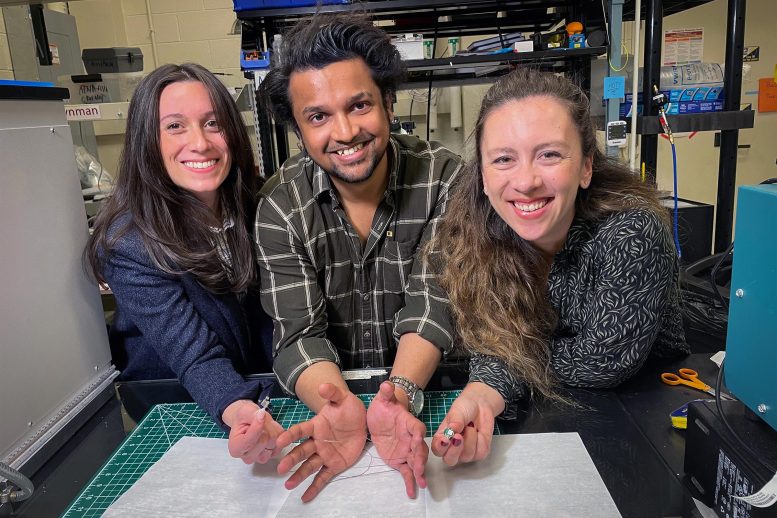
Duke University postdoc Laura Rupprecht, MIT graduate student Atharva Sahasrabudhe, and MIT postdoc Sirma Orguc in the lab. Credit: Courtesy of the researchers
As part of the center’s work, Anikeeva set out to probe the signals that pass between the brain and the nervous system of the gut, also called the enteric nervous system. Sensory cells in the gut influence hunger and satiety via both the neuronal communication and hormone release.
Untangling those hormonal and neural effects has been difficult because there hasn’t been a good way to rapidly measure the neuronal signals, which occur within milliseconds.
“To be able to perform gut optogenetics and then measure the effects on brain function and behavior, which requires millisecond precision, we needed a device that didn’t exist. So, we decided to make it,” says Sahasrabudhe, who led the development of the gut and brain probes.
The electronic interface that the researchers designed consists of flexible fibers that can carry out a variety of functions and can be inserted into the organs of interest. To create the fibers, Sahasrabudhe used a technique called thermal drawing, which allowed him to create polymer filaments, about as thin as a human hair, that can be embedded with electrodes and temperature sensors.
The filaments also carry microscale light-emitting devices that can be used to optogenetically stimulate cells, and microfluidic channels that can be used to deliver drugs.
The mechanical properties of the fibers can be tailored for use in different parts of the body. For the brain, the researchers created stiffer fibers that could be threaded deep into the brain. For digestive organs such as the intestine, they designed more delicate rubbery fibers that do not damage the lining of the organs but are still sturdy enough to withstand the harsh environment of the digestive tract.
“To study the interaction between the brain and the body, it is necessary to develop technologies that can interface with organs of interest as well as the brain at the same time, while recording physiological signals with high signal-to-noise ratio,”
Sahasrabudhe says. “We also need to be able to selectively stimulate different cell types in both organs in mice so that we can test their behaviors and perform causal analyses of these circuits.”
The fibers are also designed so that they can be controlled wirelessly, using an external control circuit that can be temporarily affixed to the animal during an experiment. This wireless control circuit was developed by Orguc, a Schmidt Science Fellow, and Harrison Allen ’20, MEng ’22, who were co-advised between the Anikeeva lab and the lab of Anantha Chandrakasan, dean of MIT’s School of Engineering and the Vannevar Bush Professor of Electrical Engineering and Computer Science.
Driving behavior
Using this interface, the researchers performed a series of experiments to show that they could influence behavior through manipulation of the gut as well as the brain.
First, they used the fibers to deliver optogenetic stimulation to a part of the brain called the ventral tegmental area (VTA), which releases dopamine. They placed mice in a cage with three chambers, and when the mice entered one particular chamber, the researchers activated the dopamine neurons. The resulting dopamine burst made the mice more likely to return to that chamber in search of the dopamine reward.
Then, the researchers tried to see if they could also induce that reward-seeking behavior by influencing the gut. To do that, they used fibers in the gut to release sucrose, which also activated dopamine release in the brain and prompted the animals to seek out the chamber they were in when sucrose was delivered.
Next, working with colleagues from Duke University, the researchers found they could induce the same reward-seeking behavior by skipping the sucrose and optogenetically stimulating nerve endings in the gut that provide input to the vagus nerve, which controls digestion and other bodily functions.
“Again, we got this place preference behavior that people have previously seen with stimulation in the brain, but now we are not touching the brain. We are just stimulating the gut, and we are observing control of central function from the periphery,” Anikeeva says.
Sahasrabudhe worked closely with Rupprecht, a postdoc in Professor Diego Bohorquez’ group at Duke, to test the fibers’ ability to control feeding behaviors. They found that the devices could optogenetically stimulate cells that produce cholecystokinin, a hormone that promotes satiety. When this hormone release was activated, the animals’ appetites were suppressed, even though they had been fasting for several hours. The researchers also demonstrated a similar effect when they stimulated cells that produce a peptide called PYY, which normally curbs appetite after very rich foods are consumed.
The researchers now plan to use this interface to study neurological conditions that are believed to have a gut-brain connection. For instance, studies have shown that autistic children are far more likely than their peers to be diagnosed with GI dysfunction, while anxiety and irritable bowel syndrome share genetic risks.
“We can now begin asking, are those coincidences, or is there a connection between the gut and the brain? And maybe there is an opportunity for us to tap into those gut-brain circuits to begin managing some of those conditions by manipulating the peripheral circuits in a way that does not directly ‘touch’ the brain and is less invasive,” Anikeeva says.
- Karlston
-

 1
1




Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.