54 million US adults may be misdiagnosed with high BP based on bad readings.
Many people may be surprised to learn the proper procedure for taking a blood pressure reading—because of how different it is from what happens during their doctor's appointments.
According to the American Heart Association and other medical experts, getting an accurate reading requires following a strict set of preparations: You must not eat, drink, exercise, or smoke within 30 minutes of a reading. You must have an empty bladder. You must sit straight up in a chair with back support. Your legs must be uncrossed and your feet must be flat on the ground. The arm to be measured must be rested on a flat surface so that it is at the same level as your heart, not lower, not higher. You must sit calmly, without talking for five minutes to relax before the reading. When it's time, an appropriately sized cuff should be wrapped around your bare upper arm, right above the elbow; it should never be wrapped over clothing. At least two readings should be taken, with the average recorded. Ideally, readings should be taken in both arms, with the highest readings recorded.
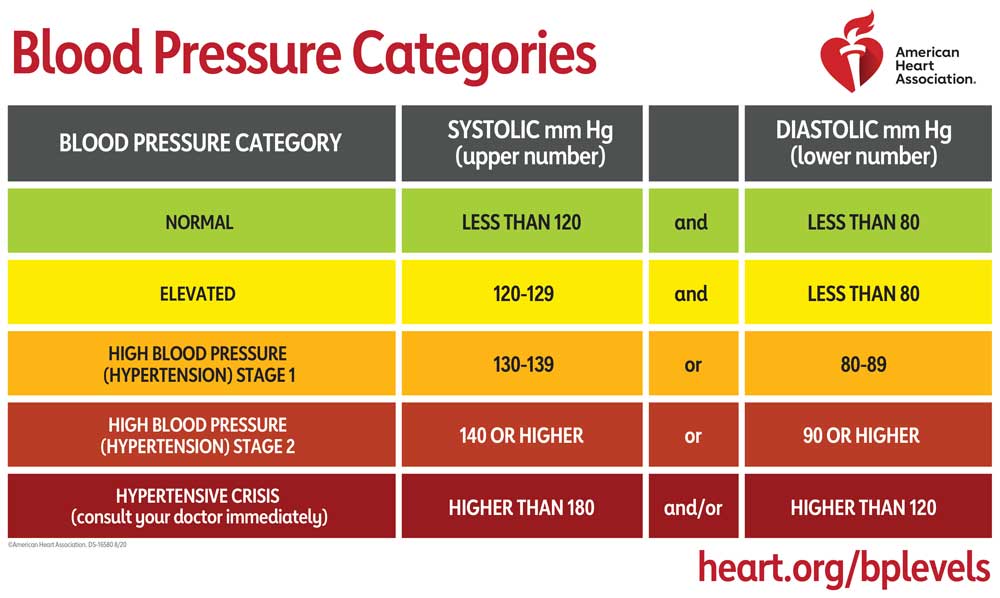
Deviations from this protocol have the potential to significantly alter your blood pressure reading—and your blood pressure category. For instance, putting the blood pressure cuff over clothing can raise your reading as much as 50 mm Hg. That's enough to make someone with early stage hypertension seem as if they're in a hypertensive crisis, at imminent risk of a stroke or heart attack. If you have to pee, the reading can be 15 mm Hg higher. Talking can raise it by 10 mm Hg.
And, according to a new study in JAMA Internal Medicine, the all-too-common practice of having your arm in a position lower than your heart can raise your systolic blood pressure reading (the upper number) between 4- and 10-mm Hg. While those numbers may not seem dramatic, they're enough to push some patients over the edges of blood pressure categories. And these inaccurate readings are thought to happen often enough that they may lead to significant overdiagnosis of hypertension. In fact, the authors of the new study—led by researchers at Johns Hopkins—estimate that as many as 54 million people in the US may be misclassified as having hypertension simply because of the way their arm is positioned during readings.
Not using the correct arm position "has the potential to lead to substantial hypertension overdiagnosis, unnecessary patient follow-ups, and overtreatment," the authors conclude.
The study echoes previous data on inaccuracies from incorrect arm positions, but goes further by investigating the most common incorrect arm positions and using a gold-standard trial design.
For the study, researchers took blood pressure readings from 133 people with a mean age of 57 years. Each person had their blood pressure measured in four arm positions—with all other blood pressure reading preparations and positioning aligned with recommendations. The four arm positions were: one, with their arm properly resting on a desk (desk 1); two, with their arm incorrectly resting in their lap; three, with their arm incorrectly down at their side; and four, with their arm properly resting on a desk (desk 2). For each position, blood pressure readings were taken in triplicate, for a total of 12 readings from each person.
Under pressure
Before participants took readings in any of the positions, the researchers had them simulate walking into a doctor's appointment. They walked for two minutes and then sat calmly in position for five minutes before taking the three readings. Before moving onto the next position, they got up and walked again and sat for another five minutes. The participants were also randomized into groups that took the first three readings (desk 1, lap, side) in different orders, with all groups ending on desk 2.
The researchers then compared the differences between desk 1 and desk 2 to differences between lap and desk 1 and side and desk 1 for each participant. The desk 1-desk 2 differences captured intrinsic variability of blood pressure reading within each participant. The comparisons to lap-desk 1 and side-desk 1 captured changes based on the improper arm positions.
In all, there was little difference in the desk 1-desk 2 comparison, with participants having a mean difference of -0.21 mm Hg in systolic blood pressure and 0.09 in diastolic. But, the improper arm positions had significant effects on the readings. Lap arm position resulted in a mean increase of 4 mm Hg in both systolic and diastolic readings. Side arm position led to systolic readings that were 6.5 mm Hg higher and diastolic readings that were 4 mm Hg higher. For those with high blood pressure readings—about 36 percent of the participants—the wrong arm position caused yet higher readings, with systolic readings about 9 mm Hg higher than desk readings.
The authors speculate that simple physiological mechanisms likely explain the increase in blood pressure when the arm is lower than the heart—more gravitational pull, compensatory constriction of blood vessels, and muscle contraction may lead to higher pressure. As for why health care providers are known to sometimes use these wrong arm positions, it may be a lack of awareness, training, equipment, and/or resources.
The authors of the study call for more training and education about proper blood pressure measurements, which are essential for appropriate management of hypertension and prevention of cardiovascular disease.
RIP Matrix | Farewell my friend ![]()
Hope you enjoyed this news post.
Thank you for appreciating my time and effort posting news every day for many years.
2023: Over 5,800 news posts | 2024 (till end of September): 4,292 news posts



3175x175(CURRENT).thumb.jpg.b05acc060982b36f5891ba728e6d953c.jpg)


Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.