Many factors may be driving an uptick of the cancer among younger and middle-aged adults
Abdominal pain is one clue something could be wrong. Changing bowel movements may be another. Other people might notice blood in their stool. Doctors may chalk that symptom up to hemorrhoids, but for some people, it’s a sign of something more insidious: early-onset colorectal cancer.
Many of the patients that Thejus Jayakrishnan sees are in their 30s or 40s, establishing themselves in their careers and perhaps settling down in a new house with young kids at home. When they find out they have colorectal cancer, they’re shocked, he says. “It’s not something you expect.” In some cases, the cancer, which takes root in the large intestine, has already spread through the body and encroached on the liver or lungs.
Though the number of colorectal cancer cases among people under 50 has been rising for decades, younger and middle-aged adults’ symptoms can still go overlooked, says Jayakrishnan, a physician at the Cleveland Clinic in Ohio. These people aren’t in the age group that doctors tend to be concerned about, he says.
That’s also been the experience of Christopher Lieu, a medical oncologist at the University of Colorado Cancer Center in Aurora. “For the last 10 years of my career, all my patients were told, ‘You’re just too young to have colorectal cancer. Don’t worry about it.’” In a June talk at the American Society of Clinical Oncology meeting in Chicago, Lieu noted that, by 2030, colorectal cancer could be the number one cause of cancer death in people ages 20 to 49. “This is a humongous issue,” he said.
In 2018, the American Cancer Society updated its guidelines to reflect the changing incidence of the disease. Screening should begin at 45 years old rather than 50, the organization now recommends (SN: 5/31/18). But younger people with early-onset colorectal cancer may still be falling through the cracks, says Yin Cao, a cancer epidemiologist at Washington University School of Medicine in St. Louis. “At least 50 percent of these cases are under age 45,” she says.
Scientists don’t know what’s driving the disease’s increase in younger adults, but they’ve been looking for answers. Recent research is beginning to reveal some hints, though the picture remains murky.
In the meantime, Cao and Jayakrishnan are looking for ways to identify the disease earlier, before it has advanced to other parts of the body. Cao’s team recently identified warning symptoms linked to the early-onset cancer. And Jayakrishnan presented a small study at the June ASCO meeting that suggests there may be metabolic differences between people with early-onset and average-onset tumors.
Science News spoke with these and other doctors about what they’re learning about early-onset colorectal cancer and what questions remain. Here are three key aspects of the disease that they wish more people knew.
More younger adults are getting colorectal cancer, a trend that’s occurring around the world.
Historically, in the United States, colorectal cancer has been a disease of older people, Cao says. But in 2017, a landmark study marked a change in who was getting diagnosed.
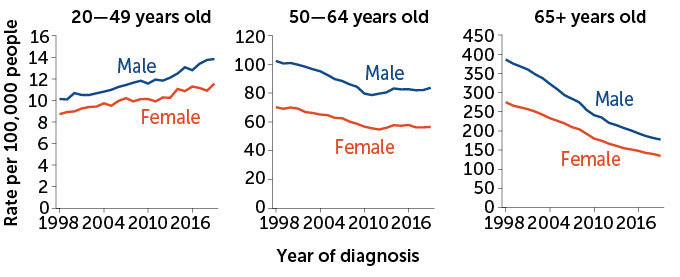
Though older individuals still made up most cases, scientists noted that, from 2000 to 2013, colorectal cancer incidence among people ages 50 to 64 had meandered downward. In people 65 and older, the rate had plunged. But there had been a 22 percent increase in cases in people under 50 (SN: 3/1/17). Whereas 59 new cases were diagnosed out of every million younger people at the start of that period, the rate had risen to 72 out of a million by the end.
“It’s really alarming because we saw this rising incidence in younger adults,” Cao says, and for a disease that hadn’t typically affected a younger population.
The data reflected what doctors were seeing in the clinic, Lieu says. Looking back through the decades, scientists can track the rise’s origin to the late 1980s. Seeing the numbers creep up for a few years might have been a blip, but “what’s concerning is that [the trend] doesn’t seem to be reversing,” Lieu says. In fact, “this problem continues to get worse.” And it appears to be occurring more or less globally. Other high-income countries, including Canada, Australia and the United Kingdom, mirror the rise.
Scientists have noticed that people born in more recent generations tend to have a greater risk of developing colorectal cancer than people born in earlier generations, what’s known as a birth cohort effect. That means someone who turns 40 today is more at risk than someone who turned 40 a decade ago, Lieu says. The pattern, and the fact that most early-onset cases lack a hereditary link, has doctors and scientists scrambling to answer a singular question: “What are younger individuals being exposed to that could account for that risk?” he asks.
Many factors may be driving the increase in early-onset colorectal cancer.
It’s not easy to take a magnifying glass to people’s lives and deduce what may be causing their disease. Sifting through a person’s diet history and past environmental exposures is complicated, Lieu says. “People have difficulty remembering what they ate yesterday, let alone their entire lives.”
That’s one reason the early-onset colorectal cancer picture is still so cloudy. Today, scientists are investigating an assortment of potential disease drivers, including obesity, antibiotics, the gut microbiome, alcohol intake, delivery by cesarean section and a diet rich in red meat and sugar.
Cao’s team, for example, has linked drinking sugar-sweetened beverages to an increased risk of early-onset colorectal cancer in women. Her group and others have also reported a connection between the disease and people with metabolic syndrome (which can include conditions like high blood pressure and excess belly fat) as well as those who eat a Western diet, among other factors.
Other teams have pointed out alterations in the gut microbiome in people with early-onset disease. They have a different community of gut microbes compared with people diagnosed later in life, a 2022 study suggested. Though many scientists are exploring the microbiome’s role in early-onset colorectal cancer, so far “nothing definitive has been determined,” says Cathy Eng, a medical oncologist at the Vanderbilt-Ingram Cancer Center in Nashville.
That seems to be true of the many potential risk factors scientists have identified. It’s also possible that younger generations are somehow more susceptible to environmental insults that kick colorectal cancer into action. “I think it’s really hard to draw a conclusion at this point,” Cao says. Lieu agrees. Scientists are still “at the hypothesis-generating stage,” he says.
Some data can even be downright confusing. One study linked oral antibiotic use with an increased risk of colon cancer yet a reduced risk of rectal cancer. “Even in the same study, you’re getting two very different answers,” Lieu says.
And the diet and obesity-related risk factors are not one-size-fits-all. In Lieu’s experience in Colorado, many of his young colorectal cancer patients are otherwise “incredibly healthy,” he says. “They’re [Division 1] athletes; they’re triathletes; they’re pretty remarkable.”
A combination of different factors working together may set off early-onset colorectal cancer, and the recipe may vary among individuals. Doctors want to be able to say, “If we stop doing this one thing, then we can prevent the cancer,” Lieu says. But, he adds, “I don’t think there’s going to be a single smoking gun.”
Four ‘red flag’ symptoms may be signs of early-onset colorectal cancer.
Though scientists have not pinned down a single, definitive cause of early-onset colorectal cancer, they have identified some early warning signs.
Up to two years before their diagnosis, people with the disease may experience abdominal pain, rectal bleeding, diarrhea and iron-deficiency anemia, Cao’s team reported in the Journal of the National Cancer Institute in May.
The researchers trawled through insurance claim data from more than 27,000 people with and without the disease. They were looking for patterns in patients’ records — telltale symptoms documented in people under 50 who were later diagnosed with the cancer. The four signs Cao’s team identified stood out because they seemed specific to early-onset cases, and they often preceded a diagnosis by months to years. Unexplained weight loss could also be a symptom to look out for, Lieu says.
Knowing and spotting the warning signs could help people get a jump on the disease. In one 2019 survey of nearly 1,200 early-onset patients and survivors, more than 7 out of 10 were diagnosed at an advanced stage of the disease, when their cancer had already grown into neighboring tissues or spread to distant locales in the body. Patients often waited months before seeing their doctor and then visited multiple doctors before receiving a correct diagnosis.
Four ‘red flag’ signs of colorectal cancer
Scientists have identified some warning signs of early-onset colorectal cancer, which can affect younger and middle-aged adults. Knowing and spotting the warning signs could help people get a jump on the disease. Four potential “red flag” symptoms are:
- Abdominal pain
- Rectal bleeding
- Diarrhea
- Iron-deficiency anemia
Many early-onset cases are actually diagnosed at the emergency room, Cao says. “The bottom line is if someone has at least two [red flag symptoms], they really need to be aware of it,” she says. “It will definitely be worth a conversation with their primary care doctor.”
Beyond noticing suspicious symptoms, other doctors are exploring different ways to spot the cancer before it spreads. In a study of 170 patients, the early-onset and average-onset diseases left different metabolic signatures in the blood, Jayakrishnan reported in June at ASCO. His team saw differences in chemical reactions involving citrate and the amino acid arginine in young people with the cancer. If Jayakrishnan’s results hold up, such metabolic signatures could one day help doctors screen people for the disease.
“If you can detect it early,” he says, “colorectal cancer has really good treatment options. It really makes a huge difference.”
One key part of early detection may simply be wider knowledge that the early-onset disease is on the rise, says Colorado’s Lieu. Most cases of abdominal pain probably won’t be cancer, he says, but “you just don’t want to ignore it.” Raising awareness of the disease and its symptoms among both patients and doctors could “save somebody’s life.”
- Kaos
-
 1
1



Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.