The UK has become the first country to approve a therapy based on Crispr gene editing, with the regulator authorizing a treatment for sickle cell disease and beta thalassemia.
The Medicines and Healthcare products Regulatory Agency has approved the therapy, called Casgevy, which was developed by Vertex Pharmaceuticals and Crispr Therapeutics. The drug could be used to replace bone marrow transplants.
The UK regulator has promised to focus on speeding the most innovative treatments to market after being given permission from next year to cut its workload by following other countries’ recommendations on approvals of other drugs. It had been struggling to keep up because of a lack of resources after the UK left the EU, where it had been a key part of the bloc’s regulatory agency.
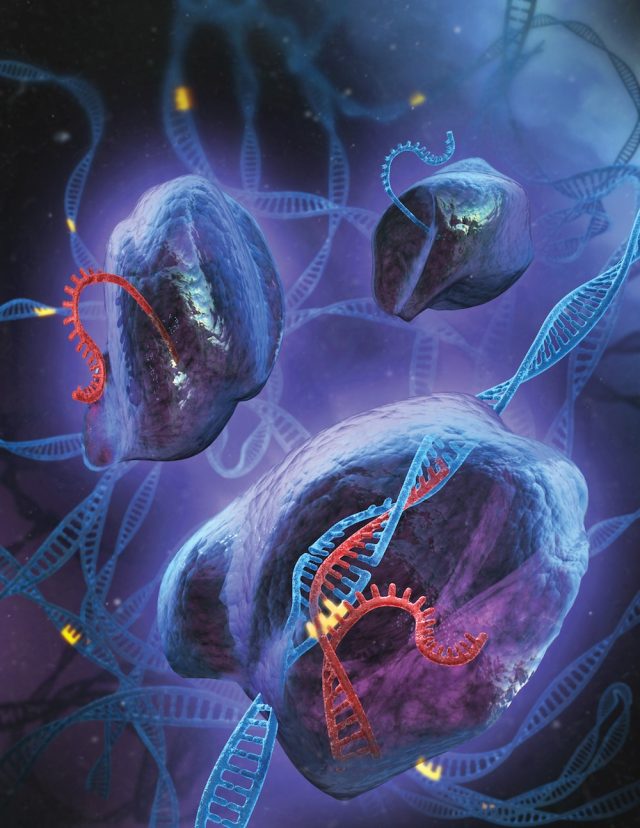
Crispr is a flexible and efficient gene editing tool based on the bacterial immune system, which has sped from the initial discovery to an approved drug in just 11 years. Scientists Jennifer Doudna and Emmanuelle Charpentier showed that Crispr could be used to disrupt, delete, or correct genetic errors in 2012, leading to a Nobel Prize in 2020.
The MHRA is hoping to attract makers of novel treatments to the UK, despite the country representing only just over 2 percent of the global drug market, far smaller than when it was part of the EU.
The UK regulator was the first in the world to approve an mRNA vaccine for Covid-19. But since the pandemic, it has been criticized for falling behind and causing delays for commercial clinical trials. It has recently caught up and restored its trial approval timelines to within the statutory limits.
In the spring Budget, UK chancellor Jeremy Hunt gave the agency an extra £10mn in funding over two years to “put in place the quickest, simplest, regulatory approval in the world for companies seeking rapid market access.”
Julian Beach, interim executive director of healthcare quality and access at the MHRA, said sickle cell disease and beta thalassemia are “painful, life-long conditions that in some cases can be fatal.” About 15,000 people suffer from sickle cell disease in the UK.
“To date, a bone marrow transplant—which must come from a closely matched donor and carries a risk of rejection—has been the only permanent treatment option,” he added.
Casgevy is a difficult drug to administer. Patients must have their stem cells extracted from their bone marrow so their genes can be edited in a laboratory. After the edited cells are put back into their body, patients need to spend at least a month in hospital before they begin to make normal red blood cells.
Crispr has been applied to blood disorders first because the cells are easier to extract to edit their genes. Other companies are working on ways to edit cells inside the body to tackle other serious genetic conditions, for example, in the eye or liver.


3175x175(CURRENT).thumb.jpg.b05acc060982b36f5891ba728e6d953c.jpg)
Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.