Last week, when we reported on the first pig-to-human heart transplant, we complained that the commercial company behind the operation wasn't more forthcoming about the genetic engineering that converted the pig into a viable donor.
We now know much more about porcine genetic engineering thanks to a new paper covering a different, more cautious test procedure. The work described in the paper is a transplant of pig kidneys into a brain-dead recipient and is meant to pave the way for trials in viable humans. The publication that describes the work contains extensive details on the genetic engineering used to ensure that the pig tissue would survive in a human host.
A test case
According to The New York Times, the recipient was rendered brain-dead by a motorcycle accident. He had signed up as an organ donor and was kept alive while his organs were screened; his next of kin gave informed consent to his body's use in the experimental procedure.
By the time the transplant took place, however, the recipient had been kept alive for five days and required blood transfusions and anticoagulants. The transplant team described his body as being in a state of severe "physiologic derangement." Ultimately, three days after the transplant, a severe hemorrhage effectively drained the body of blood and brought an end to the experiment.
The transplant was meant to parallel, to the greatest extent possible, a standard human kidney transplant. The intent was to prepare for a small clinical trial at the same facility.
The donor pig came from a facility where all animals are regularly screened for viral infections. Prior to transplantation, the recipient's serum was tested to ensure it did not contain antibodies that recognized cells from the donor. To further limit the chance of rejection, the recipient was treated with antibodies that targeted and depleted his T cells. Standard immunosuppressive drugs were then given for the remaining three days.
However, those efforts were secondary to work that was done years earlier to engineer the pig's genome so that its cells were less likely to trigger a human immune response.
The engineering
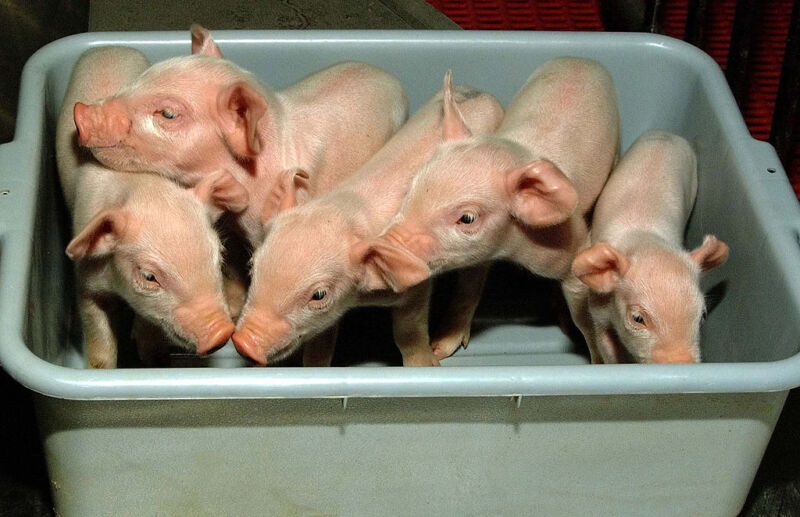
The pig itself was provided by a company called Revivicor, which also generated the donor for the pig heart transplant. These pigs have had a number of their own genes eliminated and several human genes introduced. The primary focus of these changes is to reduce the likelihood that the human immune system will recognize the pig's tissue as foreign.
Three of the pig genes that were deleted encode enzymes that attach carbohydrate molecules to proteins that reside on the surface of cells. These carbohydrate molecules are not typically essential for the function of the proteins they're linked to (more accurately, they're attached to plenty of proteins but are only important for a few). The precise arrangement of the carbohydrate molecules, however, can vary from species to species, so the molecules used by one species might be recognized as foreign by the immune system of another.
The deleted pig genes encode enzymes that generate carbohydrate modifications that aren't produced by human cells. Their elimination means the carbohydrates that they normally attach are no longer present and thus can't be recognized as foreign. For similar reasons, genes responsible for blood type were also deleted, allowing the pigs to be universal donors. A gene that encodes the receptor for a growth hormone was also deleted in order to limit the potential for the organ and/or its cells to grow uncontrollably following the transplant.
In addition, a number of human genes were added to the pig genome. Two of these genes produce proteins that inhibit something called the complement system. This system consists of a number of proteins that attach to cells that are recognized by antibodies; once there, they form holes in the membranes, killing the cell. The immune system typically uses this process to kill infected cells, but it could also kill foreign cells, such as those in a transplant.
Another gene added to the pig genome was the human version of CD47, which helps prevent the immune system from identifying and swallowing abnormal cells. The HO1 gene, which is often activated to limit the inflammatory response, was also added.
Two additional genes act as anticoagulants, which should limit the formation of clots in the transplanted organ.


3175x175(CURRENT).thumb.jpg.b05acc060982b36f5891ba728e6d953c.jpg)
Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.