In the early 20th century, the deadliest nutrient-related disease in US history ravaged the American South. Pellagra, a disease caused by a deficiency in niacin and/or tryptophan, is marked by the four "D's": diarrhea, dermatitis that leads to gruesome skin plaques, dementia, and death. At its peak during the Great Depression, pellagra killed nearly 7,000 Southerners a year. Between 1906 and 1940, researchers estimate that the epidemic struck roughly 3 million Americans, killing around 100,000.
The deadly epidemic led to voluntary—and eventually mandatory—fortification of wheat and other cereals with niacin (aka Vitamin B3). By the middle of the century, pellagra nearly vanished from the US. But, decades later, the public health triumph may be backfiring. With Americans' diets more reliant than ever on processed, niacin-fortified foods, the average niacin intake in the US is now nearing what's considered the tolerable upper limit of the nutrient, according to a federal health survey. And an extensive study recently published in Nature Medicine suggests that those excess amounts of niacin may be exacerbating cardiovascular disease, increasing risks of heart attacks, strokes, and death.
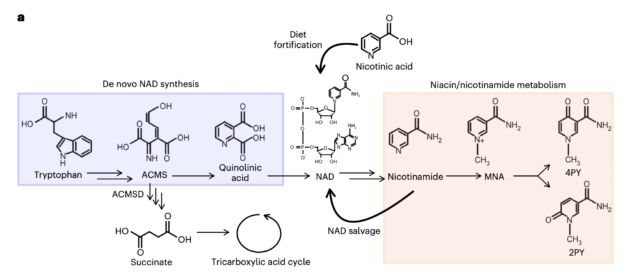
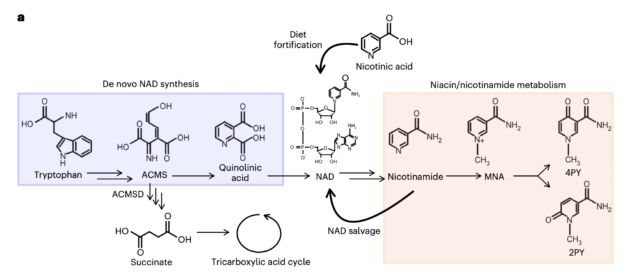
The study, led by Stanley Hazen, chair of Cardiovascular and Metabolic Sciences at Cleveland Clinic's Lerner Research Institute, connected high blood levels of a breakdown product of niacin—and to a lesser extent, tryptophan—to an elevated risk of major adverse cardiovascular events (MACE). And this elevated risk appears to be independent of known risk factors for those events, such as high cholesterol.
"What’s exciting about these results is that this pathway appears to be a previously unrecognized yet significant contributor to the development of cardiovascular disease," Hazen said in an announcement of the study. It can be measured, he added, and one day could be a new avenue for treatment and prevention.
Metabolite fishing
Hazen and his colleagues didn't start out suspecting niacin could be a culprit in cardiovascular disease. They arrived at that point after fishing through patients' blood plasma. The researchers were carefully inventorying metabolites in the fasting plasma of 1,162 patients who had been evaluated for cardiovascular disease. They were looking for anything that might be linked to a heightened risk of heart attack, stroke, or death in a three-year period that couldn't entirely be explained by other risk factors. Despite advances in identifying and treating cardiovascular disease, researchers have noted that some patients continue to be at risk of serious cardiovascular events despite having their traditional risk factors treated and controlled. Hazen and his colleagues wanted to know why.
The metabolomic trawling came up with an unknown metabolite (signature C7H9O2N2) that was significantly linked to having a MACE in the three-year period. People who had higher levels of this metabolite circulating in their systems were within the top 75th percentile for relative MACE risk in the cohort. Further work identified the metabolite as actually being two related molecules: 2PY (N1-methyl-2-pyridone-5-carboxamide) and 4PY (N1-methyl-4-pyridone -3-carboxamide)—both the final breakdown products of niacin.
Nature Medicine, 2024, Ferrell et al.
To ensure this unexpected finding wasn't some sort of blip in their cohort, the researchers looked at metabolite data from two other cohorts for validation: A US cohort of 2,331 people and a UK cohort of 832. Again, 4PY and 2PY were linked to increased risk of MACE, although when the risk assessments accounted for kidney function, 2PY was significantly linked to MACE only in the European cohort.
The researchers next turned to genomic analysis to see if any genetic changes could help explain these elevated levels. The genome-wide association study, involving data from nearly 50,000 people, linked elevated 2PY and 4PY levels to a gene that codes for an enzyme called ACMSD (aminocarboxymuconate semialdehyde decarboxylase). This is an enzyme critical in the metabolism of tryptophan, which can also lead to the production of 2PY and 4PY, though to a lesser extent than niacin metabolism. The researchers took this finding to mice, which validated the link. Knocking down ACMSD enzyme levels in mice led to elevated 2PY and 4PY levels.
They next looked for protein markers associated with one of the ACMSD genetic variants linked to high 4PY and 2PY levels, and that led them to vascular adhesion molecule 1 (VCAM-1). This is a molecule that is known to be involved in vascular inflammation, a critical component in cardiovascular disease. VCAM-1 has previously been linked to atherosclerosis, the buildup of plaques in artery walls.
The line from niacin to inflammation
The link between ACMSD and VCAM-1 was a bit of a eureka moment for the researchers, Hazen told Ars over email. The breakdown of tryptophan, where the ACMSD enzyme works, "usually accounts for a small component" of 4PY and 2PY production. But, Hazen said, "That genetic connection is what led us to the understanding of a link to vascular inflammation."
Connecting all the dots, the researchers took human cells that line the inside of arteries and veins and, in a lab, incubated them with 4PY and 2PY directly. The 4PY, but not the 2PY, induced VCAM-1 levels. When they moved to a mouse study, they saw the same. Further, the study found the initial stages of vascular inflammation in the mice after 4PY injections.
Altogether, the study suggests that the two niacin breakdown products are both clinically associated with cardiovascular disease independent of traditional risk factors, and also linked to vascular inflammation, the researchers concluded.
The study has limitations. For one, the researchers don't have any information on the dietary niacin intake of the people in their cohorts. While niacin intake is generally high in the US, Hazen noted that many factors can influence 4PY and 2PY levels, such as tryptophan breakdown. The cohorts in the study are also enriched for people with cardiovascular disease and of European-ancestry, making it unclear if all of the findings translate to people of more ethnicities and with low cardiovascular risk. The plasma samples used in the study were only single snapshots in time. Future studies should look at 4PY and 2PY levels over a longer time frame. So, in short, more work will be needed to extend and validate the findings.
As Hazen and his colleagues put it: " The present studies suggest that further investigation of the links among niacin/NAD supplementation, 4PY and atherosclerotic cardiovascular disease are needed." Those investigations could get people rethinking niacin fortification—an intervention to thwart a deadly disease that may have inadvertently spurred another.



3175x175(CURRENT).thumb.jpg.b05acc060982b36f5891ba728e6d953c.jpg)
Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.