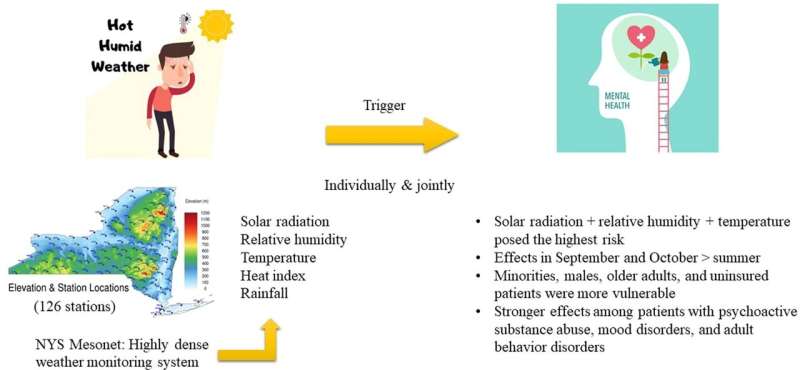
Exposure to sunny, hot and humid weather can trigger severe symptoms of mental disorders, requiring emergency care. So reports a recent study, led by researchers at the University at Albany, which used data on New York State weather and hospital emergency visits to assess how features of summer weather affect people with mental disorders.
The research was the first to evaluate combined effects of multiple meteorological factors across all classes of mental disorders designated by the World Health Organization. These findings, published in Environment International, could inform strategies to improve patient care.
Lead author Xinlei Deng, who completed his Ph.D. in May in the Department of Environmental Health Sciences at UAlbany, says, "We know that weather affects mood. But while a warm, bright day is a boost for some, others can become more easily agitated or quicker to anger. For people with mental disorders, changes in multiple weather factors can provoke symptoms that pose serious health risks."
"By examining local weather conditions together with information on emergency department visits, we found clear trends connecting high heat, humidity and sun exposure with increased emergency admissions due to mental disorders, especially among patients suffering symptoms linked to psychoactive substance use, mood disorders, stress disorders and adult behavior disorders, which can include forms of violence like pyromania. Understanding these connections can help care providers shape interventions to protect patient well-being."
The statewide analysis included two six-month study periods, focusing on the warmer months: May-October, in 2017 and 2018.
The team leveraged meteorological data from NYS Mesonet––a UAlbany-operated network of 126 weather stations in every county and borough in New York, which record atmospheric and soil conditions at 5-minute intervals. Their study looked at data on temperature, solar radiation, relative humidity, heat index and rainfall.
Emergency department visits due to mental disorders were identified using the International Classification of Diseases (ICD-10). Disorders are coded by subtype, which include categories like stress-related disorders, intellectual disabilities and intentional self-harm.
Over the study periods, 547,540 emergency department visits attributed to mental disorders were recorded in New York State. To link local weather conditions and emergency department visits, the residential address of each case was geocoded and paired with the nearest Mesonet station.
Information on patient diagnoses and demographics was obtained from the New York Statewide Planning and Research Cooperative System, a mandatory hospital discharge database covering ~95% of hospitals in the state.
Results showed that the combination of high temperature, solar radiation and relative humidity posed the greatest risk of severe mental disorder symptoms. Effects were strongest in the summer transition months of September and October. Populations impacted most acutely included: males, Hispanic and African American individuals, people aged 46-65, Medicaid or Medicare subscribers, and people without insurance.
Several mental disorder classes were distinctly responsive to certain combinations of weather conditions. For example, hospitals saw increased emergency department visits due to psychoactive substance use (e.g., consuming alcohol or opioids) when solar radiation, temperature, heat index and humidity were high. Severe symptoms of mood disorders, which include depression and bipolar disorders, coincided with less sun and high heat.
"As extreme heat becomes increasingly intense and more frequent due to climate change, we can expect these changes to have adverse physiological effects on people," said Shao Lin, senior author of the study and a professor at UAlbany's School of Public Health. "Individuals with mental disorders are especially vulnerable to these changes, and our findings suggest that multiple, simultaneous weather stressors may compound health risk. Efforts to hone targeted care must take combined factors into account."
Since mental health symptoms associated with weather can take time to manifest, the team measured "lag days" –– time between the onset of a particular weather condition and the date of hospital admittance –– to account for this delay. They found that high temperature alone presented the most immediate short-term risk, while heat index increased risk over a two-week period.
Deng, now doing postdoctoral work at the National Institutes of Health, explains, "As we learn more about the ways that weather affects mental health, putting a finer point on symptom emergence timing is critical. Understanding lag effects could help hospital caregivers know when to prepare to receive a higher number of patients in the wake of prolonged weather conditions known to exacerbate certain mental disorders."
Public health agencies like the CDC could use these findings to establish early-warning systems to preempt mental health-related violence and syndromes. Proactive measures could include facilitating access to cooling centers and encouraging patients with relevant mental disorders to pay attention to heatwaves and sun exposure, and take shelter as appropriate.
"Knowing that transition months see the highest risk of severe symptoms tells us that early warning systems and related education should start in May and continue through September-October," Lin said. "Policymakers can plan preparedness efforts using health risk thresholds connected to weather factors."
"Weather and climate have profound impacts on health –– directly from severe and hazardous weather to more indirect impacts from allergens and mental health," said Jerry Brotzge, a coauthor of the paper and the New York State Mesonet's long-time program manager who was recently hired as state climatologist in his home state of Kentucky. "Recent advances in weather observations collected at high temporal and spatial scales, like those recorded by Mesonet, have the potential to revolutionize our understanding of how changes in weather cause changes in health. Once we understand these relationships better, we can respond to patients' needs more effectively."
- Karlston
-

 1
1


Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.