It is as of yet unclear if monkeypox, SARS-CoV-2 and HIV co-infection aggravate the patient's condition.
A man in Italy tested positive for SARS-CoV-2, monkeypox and HIV all at once in July after having unprotected sex during a trip to Spain, becoming the first recorded patient to have these three viruses in conjunction, according to a new case report published in the Journal of Infection last week.
Monkeypox is spread through close contact with infectious material from skin lesions, objects contaminated with the virus, seminal fluids and secretions from the throat. Most of the cases recorded in the most recent wave of infection have been reported among men who had sex with men.
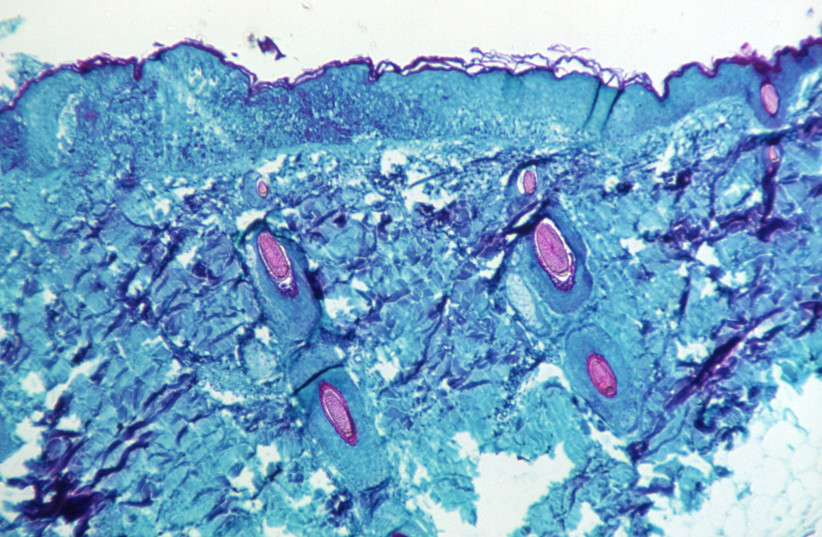
The patient in the case report, an Italian 36-year-old male, spent five days in Spain in June. Nine days after returning home from his trip, he developed a fever, sore throat, fatigue, headache and inflammation in his groin area. Shortly afterward, he tested positive for SARS-CoV-2 and within a day he developed a rash on his left arm. The day after, small, painful blisters appeared on his torso, lower limbs, face and rear.
Due to the spread of the blisters that began to evolve into pustules with a depression in the middle of them, he decided to go to the emergency room of the Policlinico “G. Rodolico - San Marco” University Hospital in Catania, Italy and was transferred to the Infectious Diseases unit at the hospital.
After being admitted, the patient reported that he had unprotected sex with men during his stay in Spain. He was tested for monkeypox and tested positive for the West African variant of the virus, which has been found to be responsible for the outbreak in Spain. Even after 20 days, monkeypox tests continued to return positive, with the physicians stressing that this could mean that patient may remain contagious for several days after clinical remission.

A student makes an AIDS red ribbon during a World AIDS Day event in Beijing, December 1, 2010 (credit: JASON LEE / REUTERS)
The patient had been treated for syphilis in 2019 and suffered from bipolar disorder, according to the case report. He had been vaccinated with two doses of the Pfizer COVID-19 vaccine in 2021 and had contracted the virus in January 2022.
Serology tests that were conducted for viral hepatitis, herpes simplex, gonorrhea, chlamydia and lymphogranuloma venereum (LGV) after he was admitted to the hospital returned negative, but he did test positive for HIV-1 with a viral load of 234,000 copies per milliliter of blood, which is considered high. His CD4 lymphocyte (a type of white blood cell) count was still average.
The scientists stressed that due to his relatively unchanged white blood cell count, it can be assumed that the HIV infection was relatively recent. A triple combination of dolutegravir, abacavir and lamivudine (medications used to treat HIV) was initiated for HIV treatment.
The patient had been treated for syphilis in 2019 and suffered from bipolar disorder, according to the case report. He had been vaccinated with two doses of the Pfizer COVID-19 vaccine in 2021 and had contracted the virus in January 2022.
Serology tests that were conducted for viral hepatitis, herpes simplex, gonorrhea, chlamydia and lymphogranuloma venereum (LGV) after he was admitted to the hospital returned negative, but he did test positive for HIV-1 with a viral load of 234,000 copies per milliliter of blood, which is considered high. His CD4 lymphocyte (a type of white blood cell) count was still average.
The scientists stressed that due to his relatively unchanged white blood cell count, it can be assumed that the HIV infection was relatively recent. A triple combination of dolutegravir, abacavir and lamivudine (medications used to treat HIV) was initiated for HIV treatment.
What did the scientists have to say?
"This case highlights how monkeypox and COVID-19 symptoms may overlap, and corroborates how in case of co-infection, anamnestic collection (case history) and sexual habits are crucial to perform the correct diagnosis," wrote the physicians in the case report.
The physicians added that sexual intercourse could be the predominant form of transmission, meaning that a complete STI screening is recommended after a monkeypox diagnosis.
Additionally, as this is the only reported case of monkeypox, SARS-CoV-2 and HIV co-infection, it is unclear if this combination aggravates the patient's condition.
"Given the current SARS-CoV-2 pandemic and the daily increase of monkeypox cases, healthcare systems must be aware of this eventuality, promoting appropriate diagnostic tests in high-risk subjects, which are essential to containment as there is no widely available treatment or prophylaxis (protection)," wrote the physicians.
- Karlston
-

 1
1


Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.