A research team led by the National Cancer Centre Singapore (NCCS) with members from Duke-NUS Medical School, KK Women and Children's Hospital, A*STAR's Singapore Immunology Network (SIgN), the University of Southampton and the Alan Turing Institute, has discovered how cancer evades the immune system and metastasizes in the body, and explores how to shut down this dangerous feature.
How cancer cells escape detection and destruction by the immune system is not completely understood, with many working to better understand it over the last few years. This latest discovery, published in Nature Communications, has implications for the development of novel strategies for cancer treatment.
The immune system searches and destroys abnormal cells such as cancer cells. However, in some instances, cancer cells avoid being detected and killed by the immune system and are able to develop and spread more easily. Metastasis, a process when cancer cells break away from the primary tumor and form in other parts of the body, makes cancer harder to treat and results in poorer prognosis.
For this reason, the team decided to investigate early onset of metastasis which typically occurs when cancer cells are detected in lymph nodes near the primary tumor.
"Like an unethical employer that forces their employees to work continuously, cancer forces the immune cells to work overtime and become exhausted, rendering them incapable of functioning normally," said Professor Gopal Iyer, senior author of the study and Head and Senior Consultant, Department of Head and Neck Surgery, Division of Surgery and Surgical Oncology, Singapore General Hospital and NCCS.
"Using a treatment to alleviate stress on immune cells, we found that immune cells were able to kill cancer cells more effectively. Still, just like some employees who are too burnt out to work properly even with a bonus, some immune cells were seen to remain exhausted even after treatment, which is how cancer may not be detected and effectively destroyed by the immune system."
Uncovering cancer immune system suppression: A three-part investigation
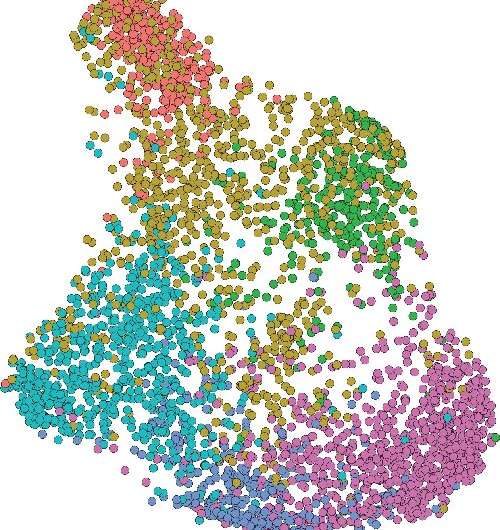
As the basis of their investigation, the team profiled primary and metastatic lymph node tumors from 14 patients with head and neck squamous cell cancers, using single cell RNA sequencing. They found pre-metastatic cells within the primary tumors with the capacity to metastasize to the lymph nodes.
They also found that a substantial proportion of CD8+ cells, a key component of the immune system that searches and kills abnormal cells such as cancer, were 'exhausted' and unable to perform their protective role. This occurred when the immune cells were repeatedly exposed to cancer and unable to eliminate it.
Next, the team identified and targeted pathways that exclusively affected cancer cells, immune cells, as well as pathways that cancer cells utilize to negatively influence immune cells, and were able to prevent some cancer spread and rejuvenate immune cells. However, despite these promising results, cancer cells continued to show their ability to escape immune surveillance.
Using a mouse model, engrafted with pre-metastatic cancer cells, the team analyzed a subgroup of CD8+ T cells expressing Midkine (MDK) receptors. One group in the model was treated with anti-PD1, while the other was a control arm.
There was an increase in exhausted MDK-receptor expressing CD8+ T cells even after anti-PD1 treatment, suggesting that the MDK-signaling pathway instigates immune suppression that undoes the effects of anti-PD1 treatment. Taken together, the results implicate MDK-signaling as a pathway which pre-metastatic cancer cells use to evade CD8-mediated immune surveillance. It also explains why some patients do not respond as well as others to anti-PD1 therapy.
Finding solutions to improve treatment outcomes
"Our investigations indicate that we can use multiple pathways to effectively treat cancer—by targeting cancer cells, the immune system and using existing therapies to counter immune system evasion by cancer cells. We know we need an increased arsenal of weapons to use against cancer and have to put it together to improve treatment outcomes," said Professor Iyer, who is also head of the Division of Medical Sciences at NCCS.
Along with exploiting the targets found in their research, the team plans to identify therapies that they can combine with anti-PD1 therapy to successfully counter CD8+ T cells expressing MDK-receptors.


Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.