A laboratory study unravels ways non-antibiotic drugs can contribute to drug resistance.
The emergence of disease-causing bacteria that are resistant to antibiotics is often attributed to the overuse of antibiotics in people and livestock. But researchers have homed in on another potential driver of resistance: antidepressants. By studying bacteria grown in the laboratory, a team has now tracked how antidepressants can trigger drug resistance1.
“Even after a few days exposure, bacteria develop drug resistance, not only against one but multiple antibiotics,” says senior author Jianhua Guo, who works at the Australian Centre for Water and Environmental Biotechnology at the University of Queensland in Brisbane. This is both interesting and scary, he says.
Globally, antibiotic resistance is a significant public-health threat. An estimated 1.2 million people died as a direct result of it in 20192, and that number is predicted to climb.
Early clues
Guo became interested in the possible contributions of non-antibiotic drugs to antibiotic resistance in 2014 after work by his lab found more antibiotic-resistance genes circulating in domestic wastewater samples than in samples of wastewater from hospitals, where antibiotic use is higher.
Guo’s group and other teams also observed that antidepressants — which are among the most widely prescribed medicines in the world — killed or stunted the growth of certain bacteria. They provoke “an SOS response”, Guo explains, triggering cellular defence mechanisms that, in turn, make the bacteria better able to survive subsequent antibiotic treatment.
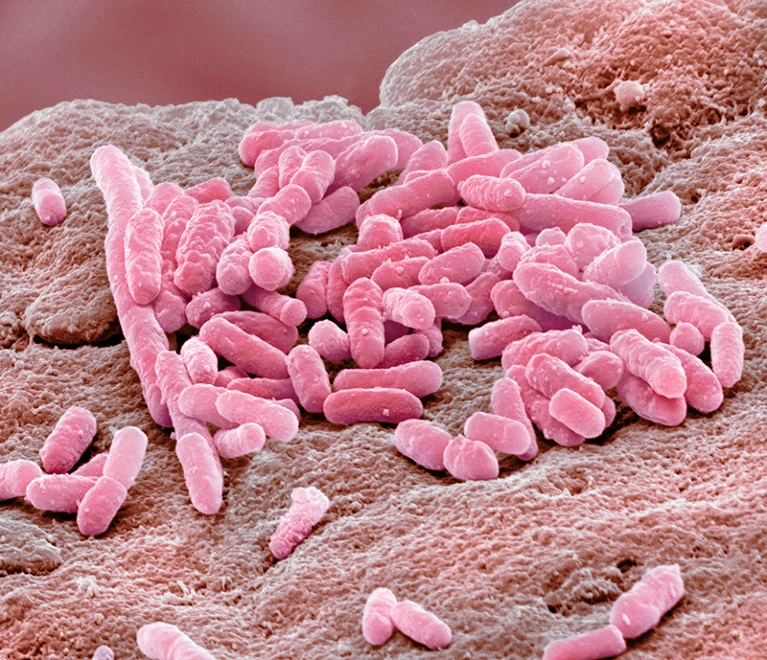
In a 2018 paper, the group reported that Escherichia coli became resistant to multiple antibiotics after being exposed to fluoxetine3, which is commonly sold as Prozac. The latest study examined 5 other antidepressants and 13 antibiotics from 6 classes of such drugs and investigated how resistance in E. coli developed.
In bacteria grown in well-oxygenated laboratory conditions, the antidepressants caused the cells to generate reactive oxygen species: toxic molecules that activated the microbe’s defence mechanisms. Most prominently, this activated the bacteria’s efflux pump systems, a general expulsion system that many bacteria use to eliminate various molecules, including antibiotics. This probably explains how the bacteria could withstand the antibiotics without having specific resistance genes.
But exposure of E. coli to antidepressants also led to an increase in the microbe’s mutation rate, and the subsequent selection of various resistance genes. Although in bacteria grown in anaerobic conditions, levels of reactive oxygen species were much lower and antibiotic resistance developed much more slowly.
Moreover, at least one antidepressant, sertraline, promoted the transfer of genes between bacterial cells, a process that can speed up the spread of resistance through a population. Such transfer can occur between different types of bacteria, allowing resistance to hop between species — including from harmless bacteria to pathogenic ones.
Growing recognition
Kiran Patil, who studies microbiome–chemical interactions at the University of Cambridge, UK, says that in the past five years there has been a growing appreciation that many non-antibiotic medicines that target human cells can also affect bacteria and contribute to antibiotic resistance. “The strength of the study is the mechanistic details,” says Patil.
Lisa Maier, who is based at the University of Tübingen in Germany and studies interactions between drugs and the microbiome, says that to understand how antidepressants can drive antibiotic resistance, researchers need to determine what molecules the drugs are targeting in the bacteria and to assess the effects of the medications on a wider variety of clinically relevant bacterial species. In 2018, Maier and her colleagues surveyed 835 medicines that did not target microbes and found 24% inhibited the growth of at least one strain of human gut bacteria4.
Patil and Maier say it is important to gather evidence to assess the real-world impact of antidepressants on resistance, such as whether antidepressants are driving the accumulation of antibiotic-resistant bacteria, particularly disease-causing ones, in people, animals or the environment.
Although significant amounts of antidepressants have been found in wastewater, reported levels tend to fall below the concentrations at which Guo’s group saw significant effects in E. coli. But concentrations of some of the antidepressants that had strong effects in this study are expected to be reached in the large intestines of people taking the drugs.
Follow-up studies
Maier says that several studies now link antidepressants and other non-antibiotic pharmaceuticals to changes in bacteria and that preliminary studies have given the “first hints” regarding how such drugs can affect the microbiomes of people taking them.
But in healthy humans, E. coli is found mainly in the large intestine, where conditions are anaerobic, meaning that the process described in the paper might not occur at the same rate in people, says Maier. Future studies should use bacterial growing conditions that model sites at which antidepressants might be acting, says Patil.
Guo says his lab is now looking at the microbiomes of mice given antidepressants. Early, unpublished data suggest that the drugs can change the animals’ gut microbiota and promote gene transfer.
But Guo and Maier caution people against stopping taking antidepressants on the basis of this research. “If you have depression, that needs to be treated in the best possible way. Then, bacteria second,” says Maier.
Although researchers and pharmaceutical companies need to quantify the contribution of non-antibiotic pharmaceuticals to antibiotic resistance, says Guo. “Non-antibiotic pharmaceuticals are a big concern that we shouldn’t overlook,” he says.
doi: https://doi.org/10.1038/d41586-023-00186-y




Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.