CAMBRIDGE, Mass. — A new wearable ultrasound patch designed to fit inside a bra could expedite the detection of breast cancer. This device is engineered to monitor breast tissue and identify tumors in their early stages, significantly boosting patients’ survival rates.
The invention comes from American researchers aiming to combat “interval cancers,” which emerge between regular scans and constitute almost 30 percent of all breast cancer cases. The survival rate for breast cancer – the most common cancer in women – is nearly 100 percent when diagnosed early. However, that figure plummets to just 25 percent for tumors detected in later stages.
The research team crafted this wearable device as a home monitoring method for those at high risk of breast cancer. The study’s lead author, Turkish scientist Dr. Canan Dağdeviren, an Associate Professor at the Massachusetts Institute of Technology’s Media Lab, is personally affected by the tragic loss of her aunt to late-stage breast cancer, was inspired to create a wearable diagnostic device that could be incorporated into a bra.
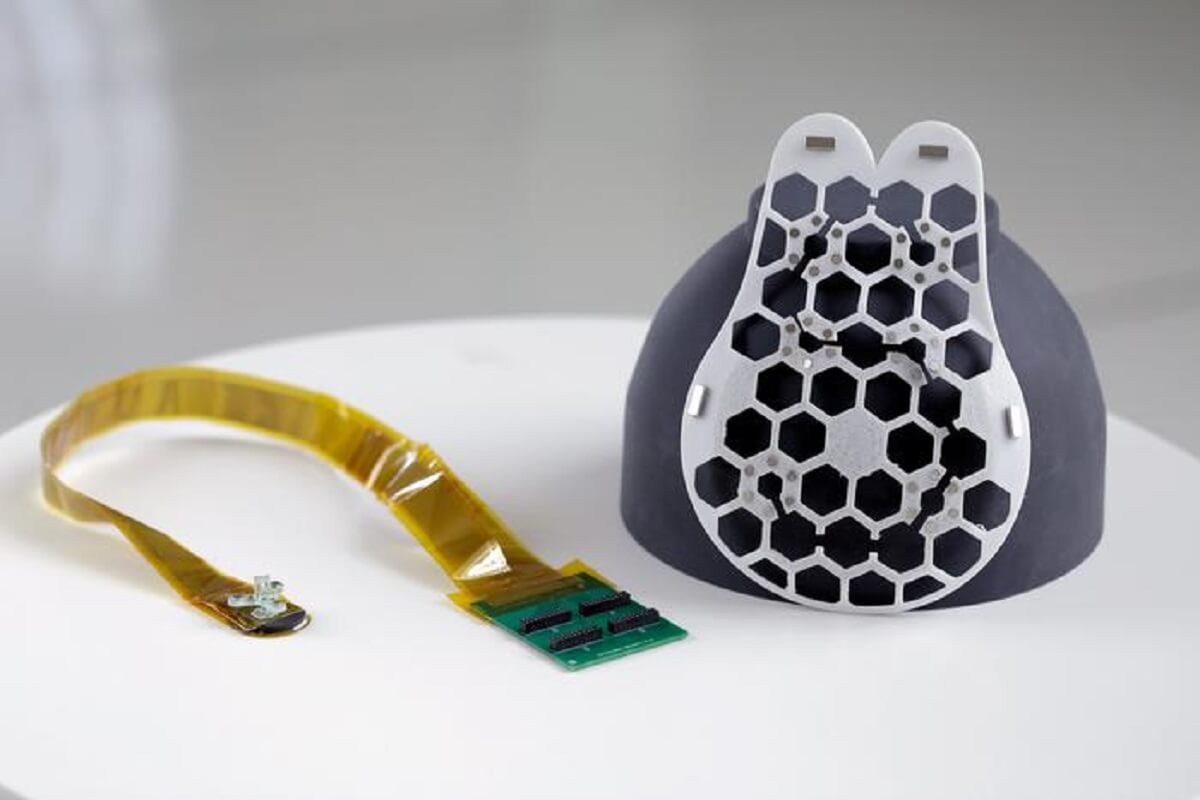
On the left of the photo, a yellow strip-cable has a green circuit board on one end, and a small ultrasound tracker on the other. On the right, the white device is teardrop shaped and has a hexagonal grid of holes where the tracker can be placed. (credit: Canan Dagdeviren)
The resulting ultrasound device aims to facilitate earlier breast cancer diagnoses in women. The device was proven to capture images as accurately as those taken at medical imaging centers. The team designed it as a flexible patch that attaches to a bra, allowing the wearer to move freely while an ultrasound tracker captures images of breast tissue from different angles.
“We changed the form factor of the ultrasound technology so that it can be used in your home. It’s portable and easy to use, and provides real-time, user-friendly monitoring of breast tissue,” says Dr. Dağdeviren in a media release. “My goal is to target the people who are most likely to develop interval cancer. With more frequent screening, our goal is to increase the survival rate to up to 98 percent.”
Interval cancers, or tumors that develop between scheduled mammogram breast screenings, account for 20 to 30 percent of all breast cancer cases and tend to be more aggressive than those detected during routine scans.

(© okrasiuk – stock.adobe.com)
To make the device wearable, the team devised a flexible, 3D-printed patch with honeycomb-like openings. Using magnets, it attaches to a bra, allowing the scanner to contact the wearer’s skin. The ultrasound scanner is housed inside a small tracker, which can move to six different positions, allowing for complete breast imaging. It can also rotate to capture images from different angles and doesn’t require specialist expertise to operate.
The device was tested on a 71-year-old woman with a history of breast cysts and could detect cysts as small as 0.3 centimeters in diameter, similar in size to early-stage tumors.
“Access to quality and affordable health care is essential for early detection and diagnosis,” says Catherine Ricciardi, nurse director at MIT’s Center for Clinical and Translational Research. “This technology holds the promise of breaking down the many barriers for early breast cancer detection by providing a more reliable, comfortable, and less intimidating diagnostic.”
Though wearers currently have to connect their scanners to a traditional ultrasound machine, the research team is working on a miniaturized imaging system about the size of a smartphone. The ultrasound patch can be reused, and the researchers envision it being used at home by those at high risk of breast cancer and those without access to regular screening.
The team also plans to incorporate advances in artificial intelligence to track how images change over time, offering more precise diagnostics. They also aim to adapt the technology to scan other body parts for early diagnoses of other cancers.
The study is published in the journal Science Advances.



Recommended Comments
There are no comments to display.
Join the conversation
You can post now and register later. If you have an account, sign in now to post with your account.
Note: Your post will require moderator approval before it will be visible.